Many people experience unusual sensations in their legs, from brief episodes of pins and needles to more persistent tingling that can disrupt daily life. Whilst temporary numbness after crossing your legs is usually harmless, ongoing tingling and discomfort in your feet and lower legs might point to a lesser-known condition called tarsal tunnel syndrome. This nerve-related problem can significantly affect your mobility and quality of life if left unaddressed, making it essential to recognise the signs early and seek appropriate medical guidance.
Understanding tarsal tunnel syndrome: what is it?
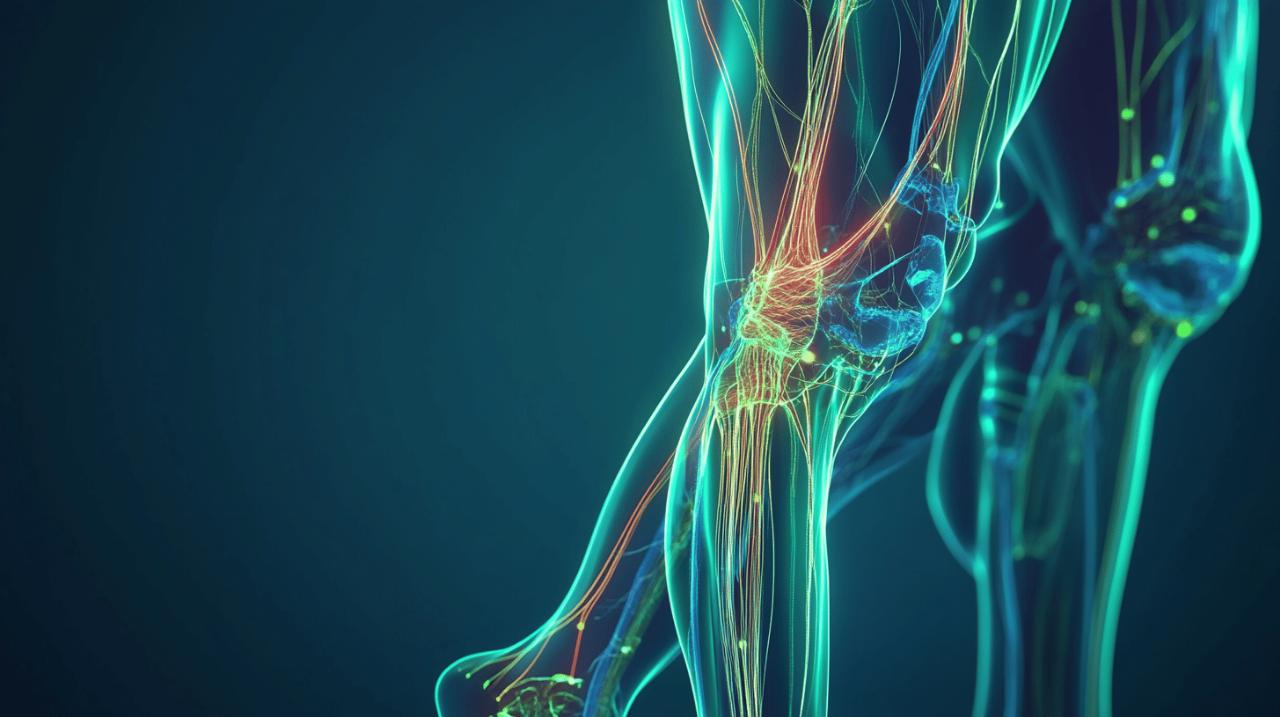
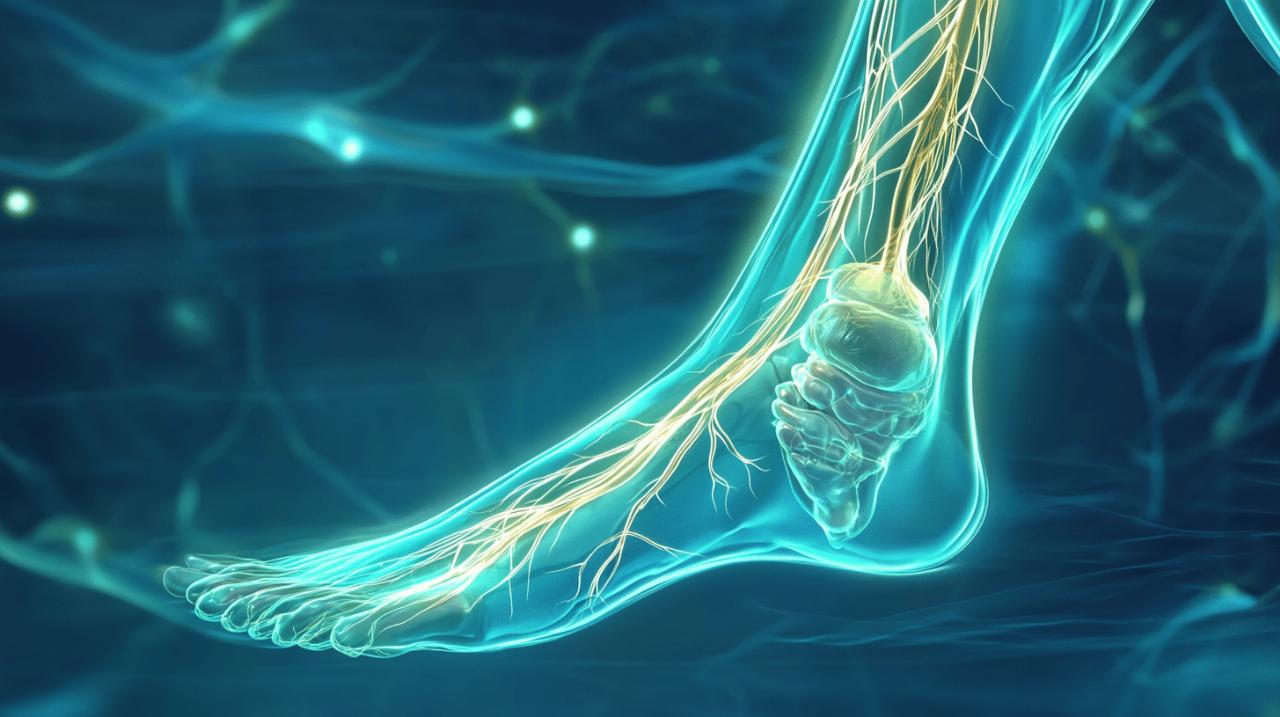
Tarsal tunnel syndrome occurs when the tibial nerve, which runs through a narrow passage in your ankle known as the tarsal tunnel, becomes compressed or damaged. This condition is somewhat similar to carpal tunnel syndrome in the wrist, but it affects the ankle and foot instead. The tibial nerve is responsible for transmitting signals to a considerable number of muscles in your lower leg, specifically around twenty-one muscles, and any interference with this nerve can lead to a range of uncomfortable symptoms. When pressure builds up in the tarsal tunnel, the nerve cannot function properly, resulting in pain, tingling, numbness, and even weakness in the foot and toes.
The anatomy behind the condition
The tarsal tunnel is a confined space located on the inner side of your ankle, beneath a band of tissue that helps hold structures in place. Within this tunnel, the tibial nerve travels alongside tendons and blood vessels, making it vulnerable to compression if the space becomes too tight. The nerve itself is crucial for sensation and movement in the foot, sending and receiving signals that allow you to feel touch, temperature, and pain, as well as enabling the muscles to contract and move your toes. Any swelling, abnormal growths, or structural changes in this area can squeeze the nerve, leading to the symptoms associated with tarsal tunnel syndrome.
How tarsal tunnel syndrome develops
There are numerous factors that can contribute to the development of tarsal tunnel syndrome. One common cause is a previous ankle injury, such as a sprain or fracture, which can lead to swelling or scar tissue that compresses the nerve. Flat feet or high arches can alter the mechanics of your foot and ankle, placing additional strain on the tibial nerve over time. Certain systemic conditions, including diabetes and arthritis, can also increase the risk of nerve compression, as these diseases may cause inflammation or changes in the tissues surrounding the nerve. Additionally, overuse from repetitive activities, such as running, hiking, or participating in sports like hockey and ballet, can aggravate the condition. In some cases, varicose veins, bone spurs, or even benign tumours in the area may contribute to the compression. It is not uncommon for the exact cause to remain unknown, but identifying any underlying factors is an important step in managing the condition effectively.
Recognising the Symptoms of Tarsal Tunnel Syndrome
The hallmark symptoms of tarsal tunnel syndrome include a range of sensations that can vary in intensity and duration. Many people describe a burning feeling or a tingling sensation on the bottom of the foot and in the toes, which can sometimes extend up into the lower leg. Numbness is another common complaint, often making it difficult to feel textures or temperatures on the affected areas. Pain may develop in the ankle, foot, and toes, and this discomfort can worsen after periods of standing, walking, or physical activity. Some individuals also experience muscle weakness in the foot, which can make it challenging to move the toes or maintain balance. In more severe cases, the muscles in the foot can become noticeably weaker, and if the condition is left untreated, there is a risk of developing foot deformities or experiencing repeated injuries due to loss of sensation and coordination.
Distinguishing tarsal tunnel tingling from other causes
It can be difficult to differentiate tarsal tunnel syndrome from other conditions that cause tingling in the legs, such as sciatica, peripheral neuropathy, or circulatory problems. However, there are some distinguishing features that may help you and your healthcare provider identify the source of your symptoms. Tarsal tunnel syndrome typically causes symptoms that are localised to the ankle, foot, and toes, rather than radiating from the lower back or affecting the entire leg, as is often the case with sciatica. The tingling and numbness tend to follow the path of the tibial nerve, affecting the sole of the foot and the inner ankle area. Unlike peripheral neuropathy, which is often associated with diabetes and can affect both legs symmetrically, tarsal tunnel syndrome may initially present on one side only. Additionally, the symptoms of tarsal tunnel syndrome often worsen with activity and improve with rest, whereas circulatory issues might cause symptoms that are more related to prolonged inactivity or specific positions.
When to Seek Medical Attention for Your Symptoms
Whilst temporary tingling after sitting in one position for too long is usually not a cause for concern, persistent or worsening symptoms should prompt a visit to your GP. You should seek medical attention if you experience ongoing numbness or tingling that does not resolve with rest, if you notice increasing pain in your foot or ankle, or if you develop weakness in your foot muscles that affects your ability to walk or stand. Other warning signs include the sensation spreading to other parts of your leg, or if you experience any changes in your ability to control your bladder or bowels, which could indicate a more serious nerve issue. Early diagnosis and treatment are crucial in preventing permanent nerve damage and ensuring the best possible outcome. If you suspect that you might have tarsal tunnel syndrome, it is important to consult with a healthcare professional who can assess your symptoms and recommend appropriate diagnostic tests.
Diagnosing tarsal tunnel syndrome properly
 Diagnosing tarsal tunnel syndrome involves a combination of clinical examination and specialised tests to confirm the presence of nerve compression and to rule out other potential causes of your symptoms. Your GP will begin by taking a detailed medical history, asking about the nature of your symptoms, when they started, and what activities make them better or worse. They will also inquire about any previous injuries to your ankle or foot, as well as any underlying health conditions such as diabetes or arthritis that might contribute to nerve problems. A thorough physical examination of your ankle and foot will be performed to check for tenderness, swelling, or deformities, and to assess the range of motion and muscle strength in your foot and toes.
Diagnosing tarsal tunnel syndrome involves a combination of clinical examination and specialised tests to confirm the presence of nerve compression and to rule out other potential causes of your symptoms. Your GP will begin by taking a detailed medical history, asking about the nature of your symptoms, when they started, and what activities make them better or worse. They will also inquire about any previous injuries to your ankle or foot, as well as any underlying health conditions such as diabetes or arthritis that might contribute to nerve problems. A thorough physical examination of your ankle and foot will be performed to check for tenderness, swelling, or deformities, and to assess the range of motion and muscle strength in your foot and toes.
Clinical examination and tests your gp may perform
One of the key tests used during the clinical examination is the Tinel's test, which involves gently tapping over the tibial nerve along the inner side of your ankle. If this tapping produces a tingling sensation or a shooting pain that radiates into your foot or toes, it is considered a positive sign for tarsal tunnel syndrome. Your doctor may also assess your foot structure, looking for flat feet or high arches, and may observe your gait to see if there are any abnormalities in the way you walk. In some cases, simple tests such as comparing the sensation and strength in both feet can help identify differences that suggest nerve compression on one side. Blood tests may be ordered to check for underlying conditions like diabetes or thyroid disorders that could be contributing to your nerve problems.
Specialist referrals and advanced diagnostic techniques
If your GP suspects tarsal tunnel syndrome based on the initial examination, they may refer you to a specialist, such as an orthopaedic surgeon or a neurologist, for further evaluation. Advanced diagnostic techniques are often necessary to confirm the diagnosis and to assess the extent of nerve damage. Electromyography, commonly known as an EMG test, measures the electrical activity of your muscles and can help determine if the nerve is functioning properly. A nerve conduction test is often performed alongside an EMG to measure how quickly electrical signals travel through the tibial nerve. If the nerve is compressed, these signals will be slowed or diminished. Imaging studies, such as an MRI scan or ultrasound, can provide detailed pictures of the structures inside your ankle and foot, allowing doctors to identify any abnormal growths, bone spurs, varicose veins, or other causes of nerve compression. X-rays may also be used to check for bone abnormalities or injuries that could be contributing to the condition.
Treatment options and management strategies
The treatment approach for tarsal tunnel syndrome depends on the severity of your symptoms, the underlying cause, and how long you have been experiencing problems. The primary goal of treatment is to relieve pressure on the tibial nerve, reduce pain and inflammation, and restore normal function to your foot. In many cases, conservative treatments can be highly effective, especially when the condition is diagnosed and addressed early. However, if conservative measures do not provide sufficient relief, surgical intervention may be necessary to prevent permanent nerve damage and to improve your quality of life.
Conservative treatments and lifestyle adjustments
For mild to moderate cases of tarsal tunnel syndrome, non-surgical treatments are typically the first line of defence. Resting the affected foot and avoiding activities that aggravate your symptoms can help reduce inflammation and give the nerve time to heal. Applying ice to the inner ankle area for short periods several times a day can help decrease swelling and numb the pain. Compression bandages or ankle braces may be recommended to provide support and limit movement that could further irritate the nerve. Anti-inflammatory medication, such as ibuprofen, can be useful in managing pain and reducing inflammation around the nerve. Custom orthotics or arch supports can be inserted into your shoes to correct any structural issues with your feet, such as flat feet, and to redistribute pressure away from the tarsal tunnel. Physiotherapy is another valuable component of conservative treatment, as it can help strengthen the muscles in your foot and lower leg, improve flexibility, and enhance your overall gait and posture. Your physiotherapist may also teach you specific stretching exercises for your feet and ankles, and advise you on proper warm-up techniques before engaging in physical activities. In some instances, steroid injections may be administered directly into the tarsal tunnel to reduce inflammation and provide temporary relief from pain and tingling. It is also important to wear supportive footwear that provides adequate cushioning and stability, and to take breaks during activities that involve prolonged standing or walking.
Surgical intervention: when is it necessary?
If conservative treatments fail to alleviate your symptoms after several months, or if you have severe nerve damage that is causing significant weakness or deformity in your foot, surgery may be recommended. The surgical procedure for tarsal tunnel syndrome is known as tarsal tunnel release or nerve decompression surgery. During this operation, the surgeon makes an incision along the inner side of your ankle and carefully releases the tight band of tissue that is compressing the tibial nerve. This creates more space within the tarsal tunnel and allows the nerve to function without restriction. In some cases, the surgeon may also remove any abnormal growths, bone spurs, or varicose veins that are contributing to the compression. The goal of surgery is to relieve pressure on the nerve, reduce pain and tingling, and prevent further damage. Recovery from tarsal tunnel surgery varies depending on the extent of the procedure and your individual healing process, but most people can expect a period of rest and rehabilitation following the operation. Physiotherapy is often an important part of the recovery process, helping you regain strength and mobility in your foot and ankle. Whilst surgery can be very effective, early diagnosis and treatment with conservative measures offer the best chance of a full recovery and can often prevent the need for surgical intervention. It is essential to follow your healthcare provider's advice and to attend all follow-up appointments to monitor your progress and to ensure that the treatment is working as expected.